Fissure doctors in Kolkata
What is Anal Fissure?
An anal fissure refers to a small tear in the lining of the anal canal, leading to discomfort, pain as well as bleeding during bowel movements.
There are two kinds of anal fissures: acute and chronic.
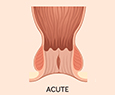
Acute Anal Fissures
Acute anal fissures are usually caused as a result of trauma to the anal canal, such as passing a large stool. They can often be treated effectively with ointments and medications within a few weeks.
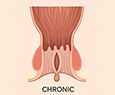
Chronic Anal Fissures
Chronic anal fissures, on the other hand, continue for more than six weeks and may be associated with underlying conditions like inflammatory bowel disease or sexually transmitted infections. These fissures usually require surgical intervention for effective treatment.
There are two kinds of anal fissures: acute and chronic.
Acute Anal Fissures
Acute anal fissures are usually caused as a result of trauma to the anal canal, such as passing a large stool. They can often be treated effectively with ointments and medications within a few weeks.
Chronic Anal Fissures
Chronic anal fissures, on the other hand, continue for more than six weeks and may be associated with underlying conditions like inflammatory bowel disease or sexually transmitted infections. These fissures usually require surgical intervention for effective treatment.
Frequently Asked Questions
Yes, while both can cause anal pain and bleeding, anal fissures are tears in the anal lining, whereas haemorrhoids are swollen veins in the rectal area.
Many anal fissures can heal on their own with proper care and lifestyle modifications. However, chronic fissures may require medical intervention.
Healing time can vary; acute fissures may heal within a few weeks with proper care, while chronic fissures might take longer and may require medical treatment.
If you experience sharp pain during bowel movement or notice blood in your stool, it could indicate the presence of an anal fissure. It’s important to schedule a doctor's appointment promptly, as untreated fissures can develop into a chronic condition. Additionally, recurring anal fissures may indicate a more serious underlying issue.
Common anal fissure symptoms include sharp pain during bowel movements, bleeding, itching around the anus, and a visible tear or crack in the anal skin.
The treatment for anal fissures varies based on their type. Acute anal fissures can often be managed with medications, while chronic fissures are more effectively treated with surgical options, such as laser fissure surgery.
Yes, maintaining a high-fibre diet, staying hydrated, practising good bowel habits, and avoiding straining during bowel movements can help prevent anal fissures.
Anal fissures can be caused by factors such as constipation, passing large stools, diarrhea or childbirth.
Diagnosis of Anal Fissure
To diagnose an anal fissure, our doctor will usually start by discussing your symptoms and medical history. They will perform a physical examination to check for visible signs of a fissure, like a small tear or crack in the skin surrounding the anus.
In certain cases, our doctor may perform a more detailed examination, known as an anoscopy, to get a closer view of the affected area. During this outpatient procedure, a small, flexible tube with a camera will be inserted into the rectum, allowing the doctor to closely examine the anus and rectum.
Additionally, our doctor may recommend further tests, such as stool samples or blood tests, to explore other potential causes of your symptoms. Once an anal fissure is diagnosed, the doctor will suggest a suitable treatment plan, which may include medications, lifestyle changes, or, in more severe cases, surgery.
Treatments for Anal Fissure By Fissure Doctors
Treatments for anal fissures depend on the severity and can be categorised into surgical and non-surgical methods.
1. Surgical treatment:
For severe cases of anal fissures, surgical intervention may be required. Anal fissure surgeries such as lateral internal sphincterotomy or fissurectomy can relieve symptoms by reducing pressure on the anal sphincter and facilitating healing. It’s essential to consult with a doctor to find the most appropriate treatment plan for your specific situation.
2. Non-surgical treatment:
These involve dietary modifications, such as increasing fibre intake and drinking more fluids to soften stools, which helps reduce straining during bowel movements. Topical medications can also aid in relaxing the anal sphincter and promoting healing.
Surgical Treatments for Anal Fissure
There are two common types of anal fissure surgery.
Open Surgery
Open surgery is a traditional anal fissure operation and it involves several key steps:
- You will receive general anaesthesia to ensure you feel no pain or discomfort during the procedure.
- You will be positioned in a particular manner to allow the surgeon easy access to the affected area.
- The surgeon will make an incision in the skin surrounding the anus to reach the anal fissure.
- The surgeon will assess the fissure to determine the extent of the damage and identify other underlying issues, if any.
- Any damaged tissue around the fissure will be removed to allow proper healing.
- Finally, the surgeon will close the incision with stitches.
After the procedure, you will be properly monitored to determine any complications and to manage any pain or discomfort you may experience.
Fissure Laser Surgery
Anal fissure laser treatment is considered to be the most effective treatment for chronic anal fissures. Here’s what to expect during the procedure:
- You will lie on the back with your hips and knees bent and your legs apart.
- The anesthesiologist will sedate you to numb the area or put you to sleep, ensuring you feel no pain or discomfort during the procedure.
- Once you are stable, the surgeon will insert a laser through the anus.
- The surgeon will guide the laser to the site of the fissure (a small tear).
- Using the laser, the surgeon will make an incision in the surrounding muscles, helping to relax the sphincter muscles.
After the procedure, you will be taken to a recovery room to rest.
Laser anal fissure surgery is recommended for individuals for whom conservative measures, such as dietary changes, stool softeners, and topical medications, have proven ineffective.
Advantages of Laser Anal Fissure Surgery
Here are some advantages of laser fissure treatment:
-
Minimally Invasive:
This procedure is minimally invasive, leading to less pain and discomfort compared to traditional surgery.
-
Outpatient Procedure:
Performed on an outpatient basis, patients can return home the same day.
-
Fewer Complications:
Laser surgery has a lower risk of complications, like bleeding, infection and blood loss, compared to conventional surgical methods.
-
Short Recovery Period:
Patients generally experience a quicker recovery, allowing them to resume normal activities sooner.
-
Highly Effective:
Laser surgery is the most effective option for treating chronic anal fissures that have not responded to conservative treatments.
-
High Success Rate:
This technique offers a higher success rate in preventing recurrence of fissures compared to traditional surgery.
-
Less Pain:
The laser seals nerve endings, resulting in reduced post-operative pain and discomfort.
-
Low Anaesthesia Risk:
This fissure rectal treatment through laser can often be performed under local anaesthesia, minimising the risks associated with general anaesthesia.
-
Minimal Scarring:
The precise incision made by the laser leads to less scarring.
Preparation for Anal Fissure Surgery
Here are some common preparation tips:
-
Follow The Surgeon’s Instructions:
The surgeon will offer specific guidelines before the surgery. Follow these instructions closely to ensure a smooth procedure and minimise the risk of complications.
-
Quit Smoking:
Smoking can affect the healing process and elevate the risk of complications. If you smoke, aim to quit at least two weeks before the surgery.
-
Avoid Blood-Thinning Medications:
Medications like aspirin and ibuprofen can increase bleeding during and after surgery. Consult our surgeon about which medications you should discontinue prior to the procedure.
-
Stay Hydrated:
Drinking plenty of water can help maintain bowel function and prevent constipation leading up to the surgery.
-
Eat a Balanced Diet:
A fibre-rich, balanced diet can help prevent constipation and reduce the risk of complications during the procedure.
-
Prepare Your Home:
Before the surgery, ensure your home is clean and comfortable. Gather any items you may need during your recovery to make the process easier.
Recovery After Anal Fissure Surgery
The recovery period for anal fissures can vary based on the type of treatment—surgical or non-surgical. Generally, non-surgical approaches may take longer to heal compared to anal fissure laser surgery.
-
Medications
Healing anal fissures with medication takes about 4 to 8 weeks. However, individual factors such as age, overall health, and the severity of the fissure can extend this timeframe. It's important to remember that medication alone may not lead to complete healing, so consulting a proctologist for an accurate diagnosis and optimal treatment is recommended.
-
Open Surgery
Recovery after open surgery usually lasts around 4 to 6 weeks, during which you may experience some discomfort and pain. Following your doctor's post-operative instructions and allowing for adequate rest can help speed up healing.
-
Laser Surgery
After laser anal fissure surgery, complete anal fissure surgery recovery time lasts for 1 to 2 weeks. Most patients can return to their normal routines within a week, making it one of the most effective treatments for anal fissures in a shorter time frame.
-
Additional Anal Fissure Surgery Recovery Tips
To support a safe recovery after anal fissure surgery, consider the following tips:- Take pain medication as prescribed by our doctor.
- Avoid strenuous activities for at least a week post-surgery.
- Keep the surgical area clean and dry to prevent infection.
- Follow a high-fibre diet to prevent constipation and straining during bowel movements.
- Drink plenty of water to stay hydrated and soften stools.
- Limit prolonged sitting, especially on hard surfaces.
- Follow our doctor’s instructions for wound care and attend all follow-up appointments.
Lifestyle changes after Anal Fissure Surgery
Making certain lifestyle changes can help relieve discomfort, ensure a safe recovery, and reduce the risk of recurrence after anal fissure surgery. Here are some key recommendations:
- Adopt a high-fibre diet to prevent constipation and minimise straining during bowel movements.
- Stay hydrated by drinking plenty of water to keep stools soft and protect the anal area from further injury.
- Limit prolonged sitting, as it can increase pressure on the rectum. Take regular breaks to stand and move around.
- Engage in light walking to improve blood circulation in the rectal area.
- Avoid heavy lifting and strenuous activities for at least 4-6 weeks following surgery to prevent unnecessary strain.
- Utilise warm compresses to alleviate pain and reduce swelling in the anal region.
- Maintain cleanliness by keeping the anal area clean and dry to prevent infections and support healing.
- Steer clear of spicy and acidic foods that may irritate the anal area and cause discomfort.
Implementing these changes will contribute to a smoother recovery and help prevent future issues.
Cost of Anal Fissure Surgery
The overall cost of anal fissure surgery can vary for each individual due to several factors, including hospitalisation fees, consultation fees for proctologists, choice of facility, insurance coverage, anaesthesia costs, anesthesiologist fees, the severity of the condition, and any required diagnostic tests.
Signs that indicate the anal fissure is healing
Here are some signs that indicate healing is taking place:
- Reduced or no pain during bowel movements.
- Decreased bleeding during bowel movements.
- Improvement in itching or irritation around the anal area.
- Smaller size of the fissure or complete closure.
- Less discomfort while sitting or standing for extended periods
- Enhanced ability to pass stool without straining or pain.
- Decreased frequency of bowel movements.
- Better digestion and nutrient absorption.
- Improved energy levels and overall well-being.
- Increased confidence in daily activities.
Importance of seeking treatment for anal fissure
Anal Fissure Diet Guidelines
Maintaining a healthy diet is always beneficial. Here are some foods to include in your diet to help relieve anal fissure discomfort:
1. High-Fiber Foods:
Incorporate plenty of fruits and vegetables to prevent constipation, which can worsen anal fissures.
2. Whole Grains:
Foods like brown rice and whole wheat bread support regular bowel movements.
3. Lean Proteins:
Options such as chicken and fish provide essential nutrients without causing discomfort.
4. Low-Fat Dairy:
Yoghurt and milk can aid digestion and contribute to overall gut health.
5. Hydration:
Drink plenty of water throughout the day to keep stools soft.
6. Nuts and Seeds:
Drink plenty of water throughout the day to keep stools soft.
7. Healthy Fats:
Olive oil and other sources of healthy fats help lubricate the digestive tract and prevent irritation.
8. Root Vegetables:
Sweet potatoes and squash provide important vitamins and nutrients without causing discomfort.
Here are some foods to avoid if you have anal fissures, as they can increase pain and discomfort:
1. Spicy Foods:
These can irritate the anal lining and worsen the condition.
2. Citrus Fruits and Juices:
These might cause discomfort and exaggerate symptoms.
3. High-Fat Foods:
Foods rich in fat can slow digestion and lead to constipation, affecting fissures.
4. Processed Foods:
Often hard to digest, these can contribute to constipation and worsen fissures.
5. Fried Foods:
High in fat, fried foods can cause digestive issues and constipation.
6. Dairy Products:
Dairy products like milk can lead to constipation, hence try to avoid them.
7. Red Meat:
Difficult to digest, red meat can contribute to constipation and worsen symptoms.
8. Nuts and Seeds:
While nutritious, consuming them in large amounts can irritate the digestive tract.
9. Spicy Items:
Items like hot sauce and chilli paste can further irritate the anal lining.
10. Alcohol:
It can dehydrate the body and lead to constipation, worsening anal fissures.
Our Patient Love Us
Get in Touch
Tell us about your disease and Dactar Babu will get the best treatment option for you.


.png)






